Access to high-quality maternity care is vital for protecting the health and well-being of pregnant women and the 3.6 million babies born annually in the U.S.
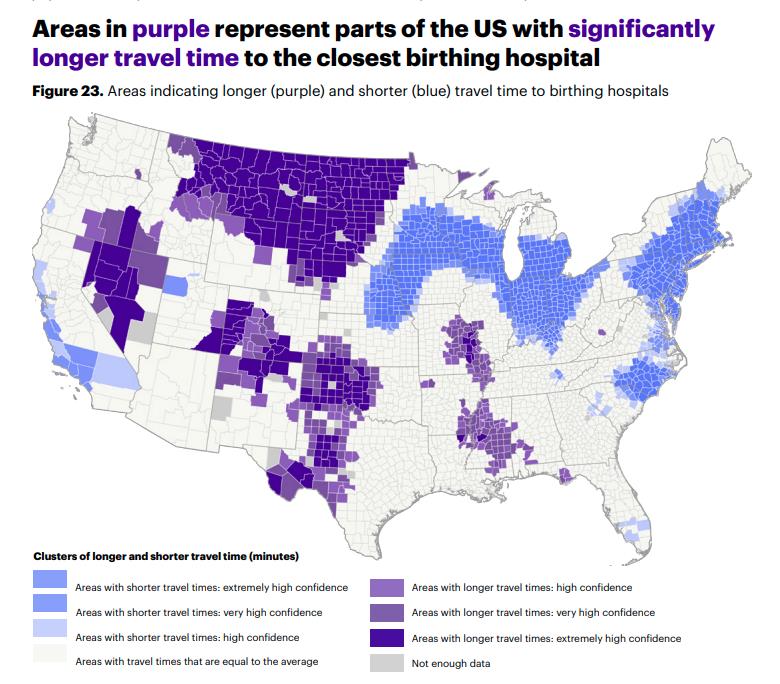
But access to maternal care isn't readily available to thousands of women across the country, especially those who live in rural areas known as maternal deserts, meaning access to maternity care is either limited or absent.
The March of Dimes 2024 Maternity Care Report, and the Future-Forward Strategies for Rural and Urban Care Delivery Challenges report from LocumTenens.com and MGMA, both highlight the harsh realities of maternal care in these regions, reasons for the lack of care and address opportunities to improve outcomes.
In this post, we’re sharing some of those findings to raise awareness of this critical issue and to provide solutions for improving maternity care in these areas.
Why are there staggering disparities in maternal healthcare access?
With nearly 70% of birth centers located in just 10 states, maternal deserts are a growing concern affecting millions of women and families across the country. In fact, an alarming 35% of U.S. counties are maternity care deserts, with more than 2.3 million reproductive-aged women living in maternity care deserts and additional 3 million live in counties with limited access.
If millions of babies are born each year, why is getting care in such a large part of the country so difficult?
A contributing factor to the lack of care is the difficulties of staffing in rural areas.
Healthcare leaders in rural settings reported their most significant challenge is with physician and APP recruitment (56%) — approximately double that of their urban (28%) and suburban (30%) colleagues. Other challenges of rural staffing include a lack of community amenities, undesirable locations and a lack of professional development opportunities. Another obstacle is that only 27 states and D.C. grant full practice authority to certified nurse midwives (CNMs); if this number was larger, there may be opportunity to staff more CNMs in some of these maternal desert areas.

The data demonstrates that where a woman lives greatly influences her access to care, as more than half of U.S. counties lack a hospital that provides obstetric care and 2.5 million reproductive-aged women live in counties without an obstetric clinician.
What is the real impact on mothers and infants?
The consequences of limited maternity care impact not only families, but also entire communities.
Rural hospital closures, shortages of OB/GYNs and midwives and difficulties in transportation result in increased difficulties and fewer options for birthing babies. In 2021 and 2022, there were at least 107 obstetric unit closures nationwide.
Limited access results in increased risks and challenges, including maternal and infant mortality, preterm birth and other major health complications. Living in a maternity care desert is also associated with a 13% risk of pre-term birth.
In addition to the more than 800 maternal deaths that occur each year, the U.S. infant mortality rate increased significantly in 2022 for the first time in two decades.
With adequate access to timely and appropriate care, many of these deaths are preventable.
What solutions are available to improve these outcomes?
As maternal deserts continue to expand, hospital systems need immediate and reliable solutions to address staffing shortages and ensure continued maternal care:
Telehealth: Comprehensive telehealth and hybrid services with skilled clinicians can make a significant impact on access to care, especially in rural areas with limited access. At LocumTenens.com, we specialize in designing custom telehealth implementation and staffing plans to provide patient care where it’s needed most.
APPs: Integral to effective healthcare delivery, APPs provide accessible care to understaffed facilities nationwide. The integration of APPs in areas lacking maternal care could be an essential tool to addressing the often-preventable issues impacting maternity care. Additionally, APPs give needed support to physicians, to help address higher levels of burnout in areas where they may be overworked.
Float pools: Optimizing float pool utilization offers many financial, patient and staffing benefits. The flexible staffing approach provided by float pools ensures patients receive timely care while reducing the strain on existing staff.
See how we successfully partnered with a rural healthcare facility to create and implement a plan to provide uninterrupted maternal careand download our recent report to learn more about how rural settings impact patient care
Getting creative with staffing solutions is one way we can address the maternal care crisis together and deliver high-quality care to those who need it most. Our women’s health team is here and ready to connect.

About the author
Heather Dauchert
AVP, Surgery Clinic
Heather Dauchert has been with LocumTenens.com for over 16 years, beginning her career as an Anesthesia recruiter in 2008 before transitioning into leadership with the Surgery Clinic team in 2019. As Associate Vice President, she now oversees all aspects of Women’s Health, Urology, ENT, and Dermatology. Growing up in an Air Force family, Heather lived around the world before settling in the South to attend Auburn University, where she graduated with honors with a degree in logistics. She later moved to Atlanta to launch her professional career. Outside of work, Heather enjoys spending time outdoors, practicing yoga, and making memories with her husband and two children.





